Female Hormones Test
Original price was: £79.£55Current price is: £55.

0% interest for 4 months with PayPal Credit. Learn more
PayPal Credit is like a credit card, without the plastic. It’s a credit limit that’s attached to your PayPal account which you can use for your online purchases. 0% interest for 4 months is available on single transactions of £99 or more. Find out more
- Add items to your Basket
- Select PayPal as your payment method at checkout
- Log into your PayPal account and chose PayPal Credit as your payment method or apply for PayPal Credit
Representive Example
Representive 23.9% APR (variable); Purchase rate 23.9% p.a (variable); Assumed credit limit £1200.
Credit subject to status. Terms and conditions apply. YorkTest acts as a broker and offers finance from a restricted range of finance providers.
PayPal Credit is a trading name of PayPal (Europe) S.á.r.l et Cie, S.C.A, 22-24 Boulevard Royal L-2449, Luxembourg.
+ FREE Delivery on all orders
Do you have irregular periods or are you wondering about your fertility? Are you concerned about your general wellbeing, energy levels, weight or mood?
Female hormone levels vary throughout the menstrual cycle, but imbalances can impact your everyday health in lots of different ways.
- Provides results for 6 key female hormone markers, including LH and FSH
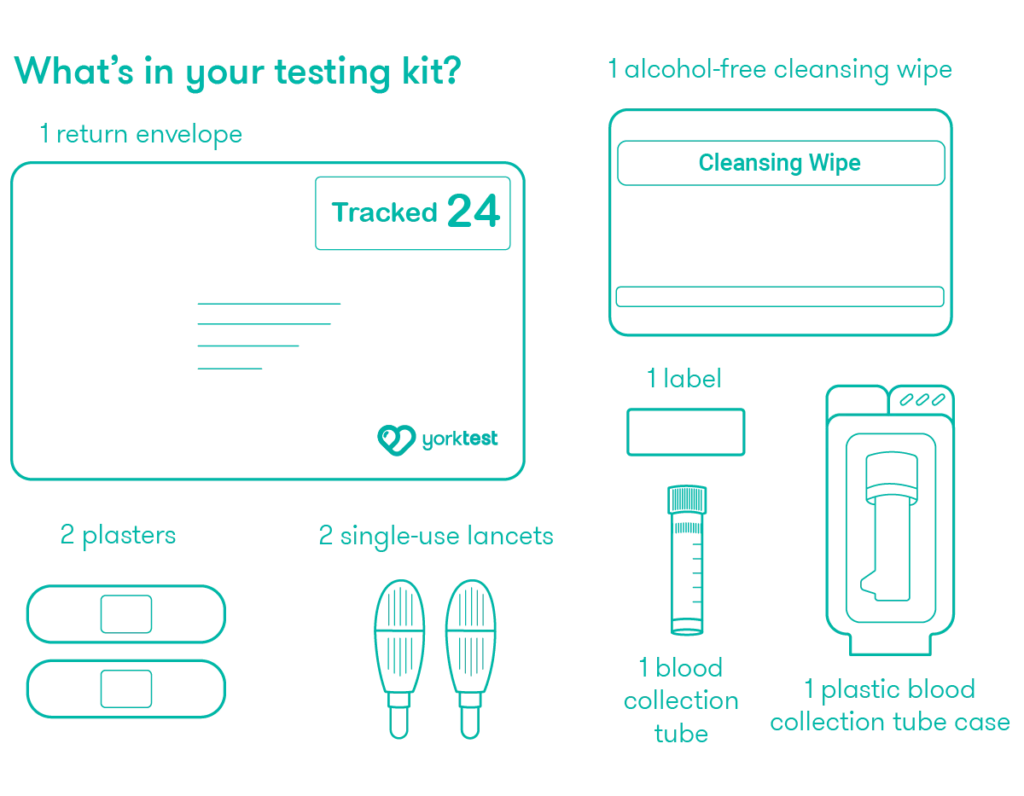
- Simple at-home finger-prick blood test. No social interaction required
- Provides hospital standard, easy-to-read results
- Provides clear information and signposting to see your GP if required
- Suitable for women aged 20 years and older; although for information about your menopause status you may prefer to take our Menopause Test
- Not suitable for those taking hormonal contraception or hormone replacement therapy
- Sample taken on Day 3 of your menstrual cycle (if cycling)
- Only available in the UK