- What is Vitamin D?
- What Does Vitamin D Do? Why Is It Important?
- Vitamin D and Calcium Relationship
- Normal Vitamin D Levels
- How Much is Too Much Vitamin D?
- Symptoms of Too Much Vitamin D
- Vitamin D Deficiency & Symptoms
- Low Vitamin D Symptoms
- Causes of Low Vitamin D
- Vitamin D Deficiency & Hair Loss
- Low Vitamin D & Weight Gain
- Vitamin D Deficiency & Neurological Symptoms
- Vitamin D SourcesÂ
- Sunlight Exposure
- Foods High in Vitamin D
- Vitamin D Supplements
- Vitamin D Supplementation
- Do Vitamin D Supplements Work?
- How Much Vitamin D Should I Take Per Day?
- When is the Best Time to Take Vitamin D Supplements?
- How to Take Vitamin D for Optimal Absorption?
- How to Test Vitamin D Levels?
- Do You Need to Fast for Vitamin D Blood Test?
- Should I Stop Taking Vitamin D Before a Blood Test?
- How to Read Vitamin D Test Results?
- References
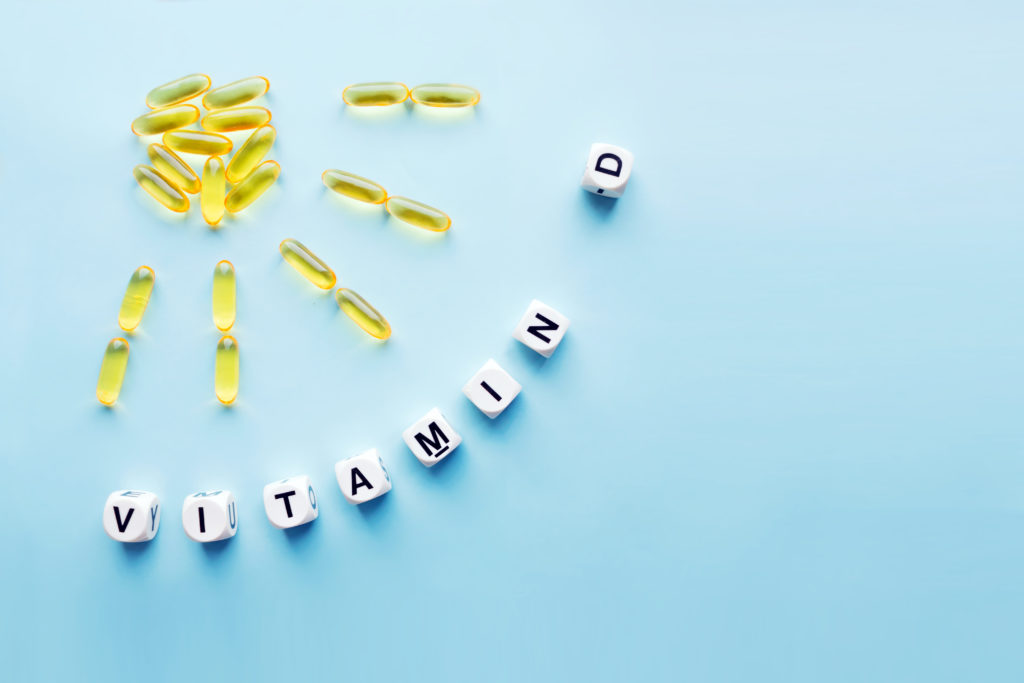
What is Vitamin D?
Vitamin D is unique from other vitamins. It’s produced in the human body naturally, it’s not found in any natural foods except egg yolks, oily fish and certain meat sources, and even when ingested from foods, the body must convert it into usable forms for it to do any good.
Also called the sunshine vitamin, vitamin D is produced in your skin naturally as a response to the sunlight’s ultraviolet B rays. It’s also available in various vitamin D-rich foods, including oral supplements. But having too high vitamin D levels can sometimes actually be a bad thing. This underscores the importance of getting a vitamin D test done and striking an optimal balance with diet, lifestyle, and supplementation, if and when necessary.
Contrary to its name, vitamin D is not technically a vitamin. Rather, it’s a prohormone, or precursor of a hormone, that’s produced photochemically in the skin. There’s a lot of chemistry unpack in understanding all that goes into vitamin D production. But essentially, vitamin D is composed of not just one but a number of biochemicals that work together to serve many biological functions.
The most natural form of vitamin D is produced photochemically in the skin from 7-dehydrocholesterol, which is a type of cholesterol precursor. Ultraviolet B (UVB) energy from the sunlight converts the prohormone to usable vitamin D3, which is then carried to the liver, then the kidneys, and eventually transformed into active, usable vitamin D.
Most vitamin D supplements use manufacturing processes that expose a plant sterol to UVB energy, thereby creating vitamin D2 which is structured very similarly to vitamin D3. Because both D2 and D3 perform nearly identical roles in the body, they are often grouped together, particularly in supplements.
What Does Vitamin D Do? Why Is It Important?
Dr Gill Hart, Scientific Director at YorkTest, explains, “There are many vital functions that vitamin D supports1. Among the most important are regulating normal immune system function and facilitating the absorption of calcium and phosphorus. Having sufficient levels of vitamin D is critical to protect against certain diseases, as well as the mineral density of bones and teethâ€.
Other biological benefits and functions that underscore the importance of vitamin D include:
- Minimising the chances of developing heart disease, flu symptoms, Covid-19 and multiple sclerosis.
- Improving mental health, regulating mood, and warding off depression symptoms.
- Reducing multiple sclerosis3 and conditions involving the central nervous system.
- Regulating weight and even aiding in weight loss, which often coincides with preventing obesity and heart disease.
- Reducing cancer risk
Vitamin D and Calcium Relationship
Vitamin D enables your body to effectively absorb calcium, and calcium is responsible for the growth and mineral density of bones. They work together to support optimal osteopathic health and ultimately maintain the integrity of strong bones. For those who may be supplementing with calcium, it could be going to waste if vitamin D levels are too low. As such, it’s important to learn how to best include these nutrients together as part of your daily routine.
Normal Vitamin D Levels
The metric of focus when measuring vitamin D levels is how much 25-hydroxy-vitamin D is found in the bloodstream. There is much debate about optimal levels with UK guidance stating more than 50 nmol/L is sufficient2. Sufficient is different to optimal levels which are typically greater than 75 nmol/L or greater than 100 nmol/L. You need to aim for optimal.
Many individuals fall below these optimal levels, especially in the northern hemisphere where we are in the UK. For people who aren’t getting enough vitamin D through sunlight exposure and/or diet, severe vitamin D deficiency can manifest, typically with levels of 25 nmol/L or less. Testing for vitamin D is important and can be tested using YorkTest’s Vitamin D Test.
How Much is Too Much Vitamin D?
Consuming too much vitamin D in supplement form over an extended period can result in an excessive calcium build-up in the body (clinically known as “hypercalcemia”). The outcome can result in weakened bones, heart problems, and kidney damage, including the formation of calcium stones.
The amount of vitamin D you need may vary seasonally depending on sunlight exposure. If you need to take vitamin D supplements because your vitamin D test shows you are sub-optimal, it’s generally recommended that 25 micrograms a day (or 1000 IU) is suitable for most people.
While it depends on the individual, very high vitamin D blood level measurements indicate too much vitamin D in one’s bloodstream. This is unusual though and more likely due to taking too much vitamin D supplementation.
Symptoms of Too Much Vitamin D
On the other end of the spectrum, too much vitamin D can have deleterious effects that manifest in many different ways. Signs and symptoms of excessive vitamin D levels, or even early stages of toxicity, include:
- Constipation
- Dehydration
- Dizziness
- Fatigue
- Frequent urination
- High blood pressure
- Irritability
- Loss of appetite
- Nausea
- Muscle weakness
- Thirst
- Tinnitus
When high vitamin D levels become toxic, more severe symptoms and reactions can occur, like hypercalcemia, kidney problems, and oddly, bone problems that manifest in ways similar to deficiency (e.g. fractures).
Vitamin D Deficiency & Symptoms
Parallel with trends in vitamin D supplementation, there has been widespread interest in studying the prevalence and health effects of vitamin D. Extensive research has been conducted on vitamin D deficiency and health implications on the musculoskeletal system as well as specific conditions involving respiratory illness, cardiovascular disease, neurological conditions, and certain cancers.
Studies have found that one in five adults in the UK have sub-optimal circulating concentrations of vitamin D but in practice this is probably an underestimate particularly in the winter. When levels continue to drop, the symptoms of low vitamin D will be far more apparent.
Low Vitamin D Symptoms
Because symptoms can vary depending on age, gender, and severity of the deficiency, low levels of vitamin D can be difficult to pinpoint unless a test is conducted. In general, the most commonly reported symptoms are:
- Fatigue or tiredness
- Bone fractures or persisting pain
- Joint pain and stiffness
- Muscle pain, cramps, and weakness
- Depression, mood changes, and irritability
- Low energy and fatigue
- Frequent illness or infections
- Anxiety
- Weight gain or weight fluctuations
- Hair loss
- Slow-healing wounds
- No symptoms as all
Causes of Low Vitamin D
Low vitamin D levels can be attributed to many different causes. In general, individuals who spend most of their time indoors or live in climates that receive very little sunlight during certain times of the year can have increased risk. People with darker skin are more susceptible to deficiency5 as their pigment naturally blocks sunlight absorption.
Not consuming enough vitamin D-rich foods can be a factor, especially among vegans who do not consume oily fish, meat and eggs, which contain the highest sources. Certain medical conditions can also play a role in causing vitamin D deficiency, such as individuals who have:
- Gastrointestinal disorders, like Crohn’s disease, cystic fibrosis, and celiac disease
- Kidney and liver diseases
- Obesity
- Weight loss surgery
Additionally, age can also play a role, which oftentimes overlaps with factors like eating a nutrient-rich diet and getting adequate exposure to sunlight.
Vitamin D Deficiency & Hair Loss
Vitamin D deficiency can contribute to many different types of autoimmune disease, including alopecia areata, or hair loss. A study found that a deficiency of vitamin D was associated with developing alopecia and that a significant number of patients who were surveyed with this condition had low levels of vitamin D6.
Low Vitamin D & Weight Gain
Compared to individuals who have a normal body mass index (BMI), people who struggle with obesity and weight gain oftentimes have low vitamin D levels7. As a result, this relationship suggests that low vitamin D levels may cause weight gain. However, few studies support a direct correlation between low vitamin D levels and weight gain. Rather, it’s a number of factors (e.g. low sunlight exposure, poor diet, insulin resistance, diabetes, etc.) that may be involved.
Vitamin D Deficiency & Neurological Symptoms
In addition to mood changes, anxiety, and depression symptoms that can be associated with vitamin D deficiency, there’s additional evidence showing that low vitamin D is cross-sectionally related to specific neurological symptoms, like impaired episodic memory and executive dysfunction, particularly involving mental shifting and processing speed.
Vitamin D SourcesÂ

Vitamin D derives from two primary sources, (1) sunlight exposure and (2) food and supplementation. One way to look at the two main sources of vitamin D is one being exogenous (deriving from external factors, like food and supplements) and endogenous (produced internally within, initiated by UVB sunlight exposure). Below we cover these main sources.
Sunlight Exposure
Regular exposure to sunlight is the most natural source of vitamin D. Although sunscreen is advised to prevent burning and other health problems associated with extended sun exposure, sunscreen can disrupt the amount of UVB absorbed through the skin. And while it’s unknown how much exposure time is required to produce the required vitamin D levels, most people are able to make enough usable vitamin D with short periods of sunlight exposure on their hands, forearms, face, and lower legs.
In the UK the best sunlight for vitamin D absorption is from late March to the end of September. But this UK sunlight is not enough though in the winter months. A related question on this subject is “can you get vitamin D from sunlight through a window?” The short answer is no; glass blocks the UVB rays needed to make vitamin D.
Certain types of UV lamps are effective in producing UVB, thereby helping to elevate vitamin D levels over time. Largely designed to reduce the depressive symptoms of seasonal affective disorder (SAD), these lamps provide a great tool for individuals who may be stuck indoors for long periods or live in regions that receive less sunlight, especially during the winter.
Foods High in Vitamin D
Unlike some vitamins found in a wide variety of foods, particularly plants, there aren’t as many foods high in vitamin D as one might think. The best sources of vitamin D come from fatty fish and fish liver oils. Smaller amounts are found in egg yolks, cheese, and beef liver.
In addition to these whole food examples, many foods and supplements are fortified with vitamin D. This fortification process is intended to add nutrients that don’t naturally occur in the product, oftentimes including vitamin A, zinc, iron, and fibre. For example, cereals, dairy milk, and most plant-based milk alternatives are fortified with vitamin D. However, some fortified foods can contain added ingredients, like sugar or hydrogenated fats. While fortified foods are quite common and can help with vitamin D intake, it’s important to know which products have unwanted added ingredients.
Among both whole foods and fortified foods, these are the sources that are the highest in vitamin D (measured by International Units):
- Cod Liver Oil – 1,360 IU (1 tablespoon)
- Trout – 645 IU (approx 35g)
- Salmon – 526 IU (approx 100g)
- Mushrooms – 130-450 IU (per 100g treated with UV light)
- Cow’s Milk – 120 IU (237ml, vitamin D fortified)
- Almond, Soy, & Oat Milks – 100-144 IU (237ml, vitamin D fortified)
- Sardines – 46 IU (2 sardines)
- Eggs – 37 IU (1 egg yolk)
- Beef Liver – 42 IU (approx 85g)
- Tinned tuna – 268 IU (approx 100g)
- Cheese – 17 IU (approx 43g, cheddar)
Most people struggle to meet their daily required vitamin D from regular sun exposure and a balanced diet, and many cases call for supplementation.
Vitamin D Supplements
Dietary vitamin D supplements can contain either vitamins D2 or D3. Vitamin D3 can be manufactured by using irradiation processes of 7-dehydrocholesterol from lanolin and the chemical conversion of cholesterol9. Vitamin D2, on the other hand, is usually produced by UV-irradiating ergosterol in yeast.
In general, most of the processes that occur in the metabolism and function of both vitamins D2 and D3 are identical. Although both forms are well absorbed in the gut, evidence indicates that vitamin D3 increases serum 25(OH)D levels (the form of vitamin D measured in the bloodstream) to a much greater extent, all while maintaining these higher levels for longer periods than vitamin D210.
Vitamin D Supplementation
As with any supplementation or treatment, it’s recommended to consult your GP, dietician, and/or nutritionist for professional guidance. Check whether you have adequate Vitamin D levels with our new Vitamin D Test. Alternatively, the YorkTest Essential Health Check includes vitamin D testing along with other key markers; it is an easy-to-use finger-prick blood test you can do from home. Vitamin D testing and evaluation ensures that any suggested supplements are taken in a careful and calculated manner.
In the world of vitamin D supplementation, some of the most common questions that arise are:
Do Vitamin D Supplements Work?
The benefits and overall efficacy of vitamin D supplementation are very positive and to be recommended.
Many studies support the efficacy of supplements in helping individuals who are deficient in vitamin D10 and do in fact struggle with real symptoms. Ultimately, the case for how well vitamin D supplements work depends on the individual, the levels they test at, and what their diet and lifestyle may look like.
How Much Vitamin D Should I Take Per Day?
The amount of vitamin D you should take per day (as a supplement) will vary depending on factors like your diet, the amount of sunlight exposure you receive, and other individual variables like age. That’s why it is important to take a test alongside measuring other important health markers. It’s also advisable to take your vitamin D results to show your GP, Nutritional Therapist or Dietician especially if you’re experiencing deficiency symptoms or eat a strict, plant-based diet. Even if you are not having noticeable symptoms, your levels might be low and you may feel a lot better for knowing your vitamin D level.
While there are many types of over-the-counter vitamin D supplements that contain very high amounts, even as high as 10,000 IU, it’s generally recommended to never exceed 4,000 IU per day, especially on a regular basis.
When is the Best Time to Take Vitamin D Supplements?
Studies on specific timing are limited, as there are very little data indicating whether it’s more effective to take vitamin D at night or in the morning. However, there is ample research showing that taking vitamin D with a meal is crucial for absorption. The bottom line in terms of timing: take vitamin D as it fits in with your routine (e.g. either breakfast or alongside dinner) and take it consistently for maximum efficacy.
How to Take Vitamin D for Optimal Absorption?
Vitamin D is a fat-soluble vitamin, so it’s most easily absorbed in the bloodstream when combined with foods high in fat. Not only is it best to take a vitamin D supplement with a meal, but pairing it with high-fat foods like avocados, eggs, nuts, and other healthy fats can improve absorption11.

How to Test Vitamin D Levels?
YorkTest’s Essential Health Check is an at-home blood test that tests for 19 different health markers, including B12 and vitamin D deficiency, cholesterol and triglycerides, liver function, and iron deficiency.
Testing vitamin D levels requires measuring the metabolised 25-hydroxy-vitamin D compound that’s present in the bloodstream. Again, this is the converted form of vitamin D that the body can use. For this reason, getting a vitamin D blood test is the only way to reliably know your levels. The two primary options are:
- Asking your GP for a vitamin D test
- Having a vitamin D test done privately, such as the Vitamin D Test
As long as tests are conducted by an accredited lab, both options can provide you with accurate information regarding your vitamin D levels and whether you need to make dietary and lifestyle changes, or consider supplementation. To help further educate you about vitamin D testing, below are frequently asked questions worth considering.
Do You Need to Fast for Vitamin D Blood Test?
Fasting is not always required for blood tests depending on what’s being measured. When fasting is required, it’s usually for 12 hours or less. YorkTest’s Essential Health Check requires fasting overnight for more than 8 hours before providing a blood sample. Fasting is not always required depending on the type of test taken. For the Vitamin D Test, no fasting is needed.
Should I Stop Taking Vitamin D Before a Blood Test?
It’s generally advised to continue taking your regular supplements and medications, even leading up to a fasted blood test. However, on the morning of your test, it’s best practice to drink only water before taking your blood sample.
It can take a day or longer for the body to metabolise the vitamin D you consume to the 25-hydroxy-vitamin D compound that’s measured in blood. In short, ceasing vitamin D intake, or taking a very high dose, won’t have much impact before a blood test.
How to Read Vitamin D Test Results?
In testing vitamin D levels in the bloodstream, the primary metric used for measuring levels is nanomols per litre (nmol/L) of 25-hydroxy-vitamin D, the metabolised version that the body can use. Fortunately, most at-home blood tests don’t require you to know basic chemistry to understand your lab results.
With YorkTest’s at-home test, you get easy-to-read traffic light results that make it simple to understand your vitamin D levels. It covers many important health markers and it’s all backed by lab-accredited testing.
While YorkTest provides accurate laboratory testing and nutritional support backed by over 40 years of experience, our tests are not a substitute for medical care but provide very valuable information.
References
1 Hart G, Furniss JL, Laurie D, Durham S. Measurement of vitamin D status: background, clinical use, and methodologies. PMID 16955631
2 https://cks.nice.org.uk/topics/vitamin-d-deficiency-in-adults/
3 Sintzel MB, Rametta M, Reder AT. Vitamin D and Multiple Sclerosis: A Comprehensive Review. Neurol Ther. 2018 Jun;7(1):59-85. doi: 10.1007/s40120-017-0086-4. Epub 2017 Dec 14. PMID: 29243029; PMCID: PMC5990512.
4 Bates B, Lennox A, Prentice A, et al. . National diet and nutrition survey results from years 5 and 6 (combined) of the Rolling Programme (2012/2013 – 2013/14). London: Department of Health, 2016.
5 Webb AR, Kazantzidis A, Kift RC, Farrar MD, Wilkinson J, Rhodes LE. Colour Counts: Sunlight and Skin Type as Drivers of Vitamin D Deficiency at UK Latitudes. Nutrients. 2018;10(4):457. Published 2018 Apr 7. doi:10.3390/nu10040457
6 Liu Y, Li J, Liang G, Cheng C, Li Y, Wu X. Association of Alopecia Areata with Vitamin D and Calcium Levels: A Systematic Review and Meta-analysis. Dermatol Ther (Heidelb). 2020 Oct;10(5):967-983. doi: 10.1007/s13555-020-00433-4. Epub 2020 Aug 9. PMID: 32772238; PMCID: PMC7477029.
7 Vranić L, Mikolašević I, Milić S. Vitamin D Deficiency: Consequence or Cause of Obesity?. Medicina (Kaunas). 2019;55(9):541. Published 2019 Aug 28. doi:10.3390/medicina55090541
8 T. A. Kalajian, A. Aldoukhi, A. J. Veronikis, K. Persons, M. F. Holick. Ultraviolet B Light Emitting Diodes (LEDs) Are More Efficient and Effective in Producing Vitamin D3 in Human Skin Compared to Natural Sunlight. Scientific Reports, 2017; 7 (1) DOI: 10.1038/s41598-017-11362-2
9 Holick MF. Vitamin D deficiency. N Engl J Med. 2007 Jul 19;357(3):266-81. doi: 10.1056/NEJMra070553. PMID: 17634462.
10 Lehmann U, Hirche F, Stangl GI, Hinz K, Westphal S, Dierkes J. Bioavailability of vitamin D(2) and D(3) in healthy volunteers, a randomized placebo-controlled trial. J Clin Endocrinol Metab. 2013 Nov;98(11):4339-45. doi: 10.1210/jc.2012-4287. Epub 2013 Sep 3. PMID: 24001747.